Stopping Alzheimer's occurring
Interview with
Scientists in Ireland may have found a new way to stop an individual developing 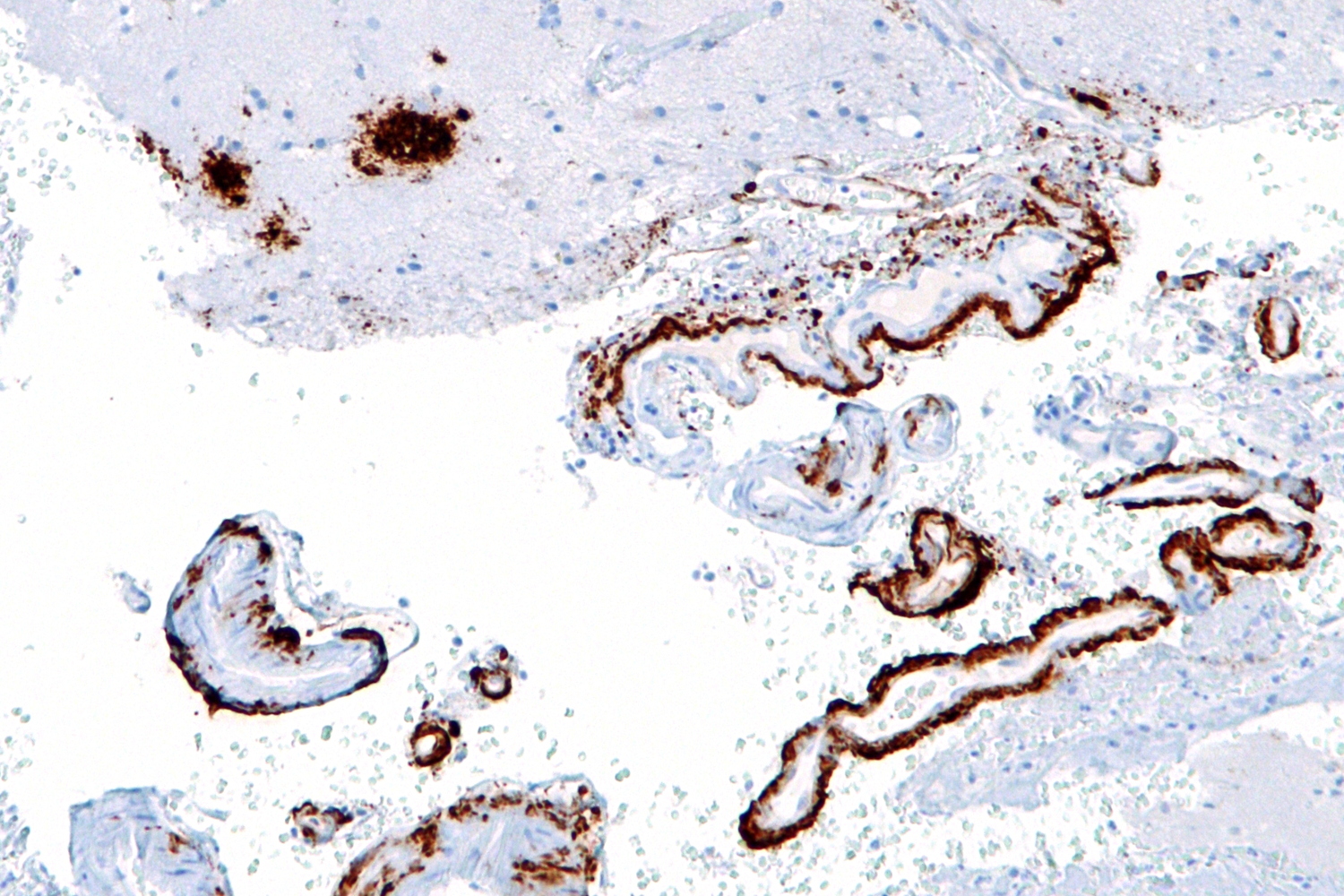 Alzheimer's Disease. Alzheimer's occurs owing to a build up in the brain of a toxic material called amyloid beta, which kills nerve cells. Reducing the levels of amyloid beta in the brain should therefore cut the risk of Alzheimer's occurring. Researcher Matthew Campbell has found a way to do this by deactivating two molecules - called claudin-5 and occludin - which control the "blood brain barrier". Temporarily disarming the barrier allows the beta amyloid to be carried away harmlessly in the bloodstream. He explained his findings to Chris Smith.
Alzheimer's Disease. Alzheimer's occurs owing to a build up in the brain of a toxic material called amyloid beta, which kills nerve cells. Reducing the levels of amyloid beta in the brain should therefore cut the risk of Alzheimer's occurring. Researcher Matthew Campbell has found a way to do this by deactivating two molecules - called claudin-5 and occludin - which control the "blood brain barrier". Temporarily disarming the barrier allows the beta amyloid to be carried away harmlessly in the bloodstream. He explained his findings to Chris Smith.
Matthew - In our brains at the moment, we are producing amyloid beta and it's able to get out of the brain via the blood-brain barrier. Something is happening in Alzheimer's disease that is preventing this material from getting out of the brain. In patients who have Alzheimer's disease, this material builds up to such an extent that it eventually begins to kill brain cells. If they're the cells that allow you to make memories, that allow you store memories, well then those memories would be gone forever and they won't come back.
Chris - What do you think is governing that process then and why does it go wrong?
Matthew - In all our blood vessels in our body, there are cells that we term 'endothelial cells'. There are specific - what we term 'receptors' on the endothelial cells and what these receptors do is they allow for material to remove from brain to blood and blood back into the brain. Now, in ageing, we lose the potential to be able to transfer this material from brain into blood and blood into brain. And some people for whatever reason, we still aren't fully certain, are more susceptible to these processes slowing down.
Chris - So, what have you found now that might influence that process?
Matthew - What we've discovered for the first time is that this molecule - amyloid beta - itself can open up these junctions between endothelial cells and facilitate its own movement from brain back into blood.
Chris - How does the amyloid beta open up the blood-brain barrier?
Matthew - In effect, what we've discovered is that amyloid beta can itself decrease the levels of these two components. One of them is called claudin-5, the other one is called occludin. These components hold endothelial cells together very, very tightly. If we can now go ahead and design drugs that specifically target these molecules, it could lead to a therapy that could allow for the clearance of amyloid beta from brain to blood in the context of Alzheimer's disease.
Chris - Summarising that then, the brain makes amyloid beta. Normally, this would exit harmlessly into the bloodstream. It probably is doing that, you're saying because it stimulates the blood-brain barrier to open up a little bit for some reason this process goes wrong in people who are destined to develop Alzheimer's disease. But if we could crowbar-open the blood-brain barrier again, we might be able to encourage this stuff to come back out of the brain. It wouldn't accumulate and that should stop someone developing Alzheimer's disease at such a high rate as they would've done.
Matthew - Exactly. So, what we need to do when we're thinking of therapies is to get in pre-emptively before the damage has gone to such an extent that the cells that we're trying to preserve have actually died.
Chris - How do you know this is going to work?
Matthew - We have mice that have genes that cause Alzheimer's disease. So, we have shown in these animals that we control claudin-5 and occludin levels. Over time, we can decrease the levels of amyloid beta in their brains and lead to better cognitive performance in these mice as well. We also recently have data from a non-human primate study whereby we've shown that the molecule that we use that targets these molecules, claudin-5 and occludin, is very, very safe when it's administered into a vein of a larger animal such as a non-human primate. So, it gives us a lot of hope that we're on to something here that this could be a new form of therapy for Alzheimer's.
Chris - Is there not though a potential risk of there being a problem because the blood-brain barrier is being rendered deficient or defective by what you're doing?
Matthew - It's a really, really good point and it's something we have to be very, very acutely aware of as we move towards clinical deployment of this. But we've dosed some animals for up to a year with the material that modulates the blood-brain barrier. There's very, very limited effects in the animals. The safety profile of this approach is very, very strong. So, we have a lot of hope that it's actually quite safe.
Chris - It's very encouraging, isn't it? That was Matthew Campbell from Trinity College Dublin, describing the study that he's published this week in Science Advances.










Comments
Add a comment