AI and immunotherapy: The cutting edge of cancer research
Today, we turn our attention to cancer. With several high profile cases in recent weeks, we look at the broader picture across the UK as of late. Then, the mechanisms by which cancer takes hold of its host, before we explore recent innovations helping to combat cancer: AI screening programmes and precision medicine show particular promise...
In this episode

00:42 - Cancer diagnoses trending upwards in the UK
Cancer diagnoses trending upwards in the UK
Jon Shelton, Cancer Research UK
King Charles, recently diagnosed with cancer himself, is now the patron of Cancer Research UK: the world's leading independent cancer charity. We thought we’d put in a call to them to talk us through the latest trends and statistics in this country. Jon Shelton, head of cancer intelligence at Cancer Research UK, spoke with Chris Smith…
Jon - It's a bit of a mixed picture, really. We have an ageing and growing population, so the number of new cases that we are seeing each year is increasing. Currently, we see about 375,000 new cancer cases diagnosed every year across the UK, but we project that this is going to rise over the coming years, up to around half a million cases per year by 2040. But when we account for the changing population, it's more useful to look at age standardised rates, and we're starting to see signs of falling after seeing it rise to a peak in about 2012 about 10 years ago. This is very much influenced by the largest four cancer sites: breast, lung, colorectal, and prostate cancer. These four cancers themselves account for just over half of all cancers. If we take those cancers out, overall rates over the last 25 years have been pretty steady. There's lots of different reasons and causes behind trends in each one. Lung cancer, for example, has been falling for men for decades and only more recently for females, but that's very reflective of historical smoking prevalence. There's different things that are happening, more we can do, and things like smoke-free legislation, which will help accelerate this decrease over coming years.
Chris - In summary, we're seeing a downward trend in rates of cancer among younger people but, because we have an ageing population overall, we still see enormous numbers of cancers. In some respects, some reasons to be quite pleased because we are seeing those improvements which probably also reflect a number of lifestyle factors, doesn't it? With reduced smoking rates, perhaps better living conditions which are helping a bit. But what are jumping out as the main concerns for you? Are there any areas where things are not going in the right direction?
Jon - As I said, it is a mixed picture. We are seeing increases in some sites such as liver cancer, kidney, thyroid (which have seen jumps of about 25% over the last decade.) Generally, these are smaller cancer sites, but any of these sites that are showing this change, we really need to understand what's happening. That's the importance of research, understanding what's the cause behind these changes? Is it associated with preventable risk factors? Are there genetic links? What's really causing this growth in these cancers? As we make progress with, say, smoking, there are other areas like overweight and obesity which is the largest preventable risk factor after smoking. Relatively speaking, we've got a high prevalence of overweight and obesity in the UK compared to other European countries. There are other concerns that we have as well. We're seeing increases in some cancer sites in earlier ages, colorectal cancer of about 30% over the last decade in people under 50. Some of that might actually be because of better awareness of symptoms. It might be about better diagnosis: we've got the faecal immunochemical test (FIT) which is used for screening but can be used in younger people who present at their GP with symptoms. But it also can be more concerning aspects. For example, changes in our diet. This leads to changes in bacteria in our gut. Again, it's that research that's really important: understanding what is causing these changes, what is causing these increases so that we can try to understand and try to reverse the trends we are seeing.
Chris - Are you referring here though to cases, modalities, or both? In other words, if we're seeing more cases of cancer, that's a worry, but if we're much better at picking them up and dealing with them and curing people, then that's arguably a reason to be very pleased.
Jon - So, mortality rates, we have seen some really good progress. Cancer survival, for example, has doubled and this therefore is reflected in mortality. Yes, we might be diagnosing more people, we might be seeing that slight increase in rates, but we have seen this reduction in mortality. It's about 1% per year over the last decade. For example, in that 35-69 year-old group, we've seen a reduction of about a third over the last 25 years, which is fantastic progress and we've seen that over a lot of cancer sites. But despite these improvements, there's still a lot more to go. We've still got around one in four deaths in the UK caused by cancer. We've really got to focus on how we can reduce cancer mortality, whether that's through prevention, whether it's through early detection and diagnosis, or indeed developing those new treatments to help improve outcomes for patients when they are diagnosed with it.
Chris - Presumably it does help when high profile people talk about their diagnosis and their treatment and so on. That must also stimulate behavioural change in the population around risk factors, but also maybe make people more disease aware so they are more likely to avail themselves of screening opportunities and so on?
Jon - It's always sad to hear the news of anyone diagnosed with cancer and a cancer diagnosis is one that can be difficult to share with family and loved ones, let alone the public. But when well-known figures do share that cancer diagnosis it leads to a much greater awareness of cancer in general. This can lead to positively affecting people's behaviour. When Jade Goody, for example, was diagnosed and very sadly died with cervical cancer, the discussion in public led to a much larger uptake of cervical screening, which was hugely positive coming out of such a sad story. We've seen it with Dame Deborah James in her discussions and being so clear in her communication about her bowel cancer which didn't just raise awareness of bowel cancer, but of cancer in general and gave strength to so many people in going through that diagnosis and treatment. And we're seeing it more recently: we've had the King and Princess announcing bravely, sharing the news of their cancer diagnoses this year. It leads to that discussion, that greater awareness about cancer and reinforces those messages that we can give to people that you know your body best and reminding people to seek help from their doctor if there's a change in their body that does concern them.
06:54 - How cancer hijacks healthy cell functions
How cancer hijacks healthy cell functions
Giulia Biffi, CRUK Cambridge Centre
What’s actually going on inside the body when a cancer forms? What is driving the disease, how does it subvert our normal healthy systems, and how does it begin in the first place? Chris Smith went to see Cancer Research UK Cambridge Institute’s Giulia Biffi…
Giulia - Cells in a normal tissue maintain the structure and function of the tissue by either expanding through a process called cell proliferation or by reducing in size through a process called cell death. Cancer hijacks these two processes leading to increased proliferation or impairment of cell death.
Chris - Why does that happen in the first place, though? What changes to make the cells begin to behave like that?
Giulia - One mechanism that leads to cancerous growth is through mutations in genes that are components of the DNA, which is the blueprint of a cell that tells a cell, you are a lung cell, or a liver cell, or a skin cell. Typically, mutations occur in two different types of these genes. One set of genes, for example, has as a function suppressing the growth of the cancer and has a role in cell death. Those are called tumour suppressor genes. Then, the other set of genes are called oncogenes. Those genes acquire mutations that lead to hyperactivation of signalling downstream. So the cancer would grow, but also the cancer can reprogramme cells of the normal organ and reprogramme them in a way that would support its growth and also spread it to other organs. It's a crosstalk relationship between these two different components.
Chris - That's intriguing. So the cancer cells can get non-cancerous cells to start to help them. It's almost like in a war you persuade the local population who are not in theory on your side to start helping the enemy?
Giulia - Yeah. The cancer cell can either prevent some cells from doing their function in fighting the cancer or can encourage other cells, other normal cells, to help further proliferate or disseminate to other sites.
Chris - Do they do that by 'talking' to the cell next door by reaching out and touching it? Or is that because they send chemical signals? Or both?
Giulia - It's actually both. There can be communication via cells through secreted factors, or there can be communication via cell-cell interactions that would lead a cell to, for example, migrate or invade a blood vessel and then colonise a different organ.
Chris - And presumably, if this is going on, it can also frustrate our efforts to treat the tumour because it could limit access of drugs to the cells you want to kill or other things that would normally control cell growth can be prevented?
Giulia - Yeah, so access to drugs can be a problem also because cells that are not the cancer cells could uptake those drugs and this would reduce the concentration of the drug and wouldn't affect the cancer as well as if those cells weren't around.
Chris - What about when the cancer spreads to a distant site, though, in the body? Because I remember being really struck by a paper published in one of the big science journals a few years ago showing that before a cancer spreads to, say, the lung, you can see that the cells in the lung start to change their behaviour and even bring in other cells from other bits of the body that are not cancerous and then the cancer spreads. It's like a bird making a nest remotely that it then moves into?
Giulia - If you can imagine a cancer growing in a particular organ, it will affect the function of that organ. But also that will affect systemically the whole host, the whole person. Other organs may also be reprogrammed from a distance by the cancer in a different organ. The cancer would benefit from these changes and be better able to grow in that different organ.
Chris - So we've got local effects where the tumours are growing, they're expanding, putting pressure on tissue and that can do harm. They're subverting local tissue into changing its behaviour, which can do harm and also stop drugs doing their job. They can also do that at remote sites in the body by understanding that malignant process. Does that give us clues as to how we might have an 'in' to try and tackle cancer?
Giulia - Intrinsically, some cancers are more dangerous than others but, broadly speaking, cancers are more dangerous when they are at a late stage of development: they have already spread to other organs. You can imagine that if you have a cancer that's localised to one organ, it could be more easily treatable. For example, it could be surgically resected, removed. But if the cancer is in multiple organs it's much more difficult to target. If we are, for example, to identify this cancer at earlier stages with early detection strategies, then we already have a better window in which we can intervene with the patient and help them.
Chris - Are there any clues that are emerging from research like yours, though, that tell us new ways that we might be able to combat cancers.
Giulia - Therapeutically, well, by better understanding how these cancer cells are talking to the normal tissue and reprogramming it to support its growth and spread into other sites, then we will be able to target those interactions and more effectively design treatments that are targeting multiple tumour promoting effects.
Chris - When a person gets cancer, by the time they're diagnosed with, say, a pancreatic cancer like you work on, how long have they probably had that disease for before it takes off and becomes clinically manifest and they're off to the doctor?
Giulia - Cancers may have different windows from when they start arising until they are diagnosed, but typically it's years. I think there is a really big window of opportunity if we were to identify ways to detect it earlier. In addition to early detection, methods that are preventative are also good strategies. For example, colonoscopies, endoscopy procedures that would identify precancerous lesions that can be removed, those are effective, even more effective than early detection strategies. For example, here in Cambridge, Professor Rebecca Fitzgerald has designed and implemented the cytosponge that allows us to identify our oesophagus, which we can treat and intervene on, and then these patients wouldn't then progress to oesophageal cancer.

14:17 - Cancer screening programmes improved by AI
Cancer screening programmes improved by AI
Gerald Lip, University of Aberdeen
‘Prevention being better than cure’ is not a new idea, and so it’s no surprise that, with cancer being the leading cause of death in the UK, spotting signs of the disease early is a crucial part of the plan to improve patient outcomes. So, how can we do that, and how are scientists trying to harness new technologies to stay one step ahead of cancer? Gerald Lip is the clinical director of breast screening in the north east of Scotland and a senior lecturer at the University of Aberdeen…
Gerald - Screening is the process where we look at healthy people, people who have no symptoms, and we test them to see if they have any disease. For instance, in breast screening, women will come, they don't have any breast lumps, they don't have any problems, they're between the age of 50-70, and every three years they will come and have a mammogram done. Then, we look for any signals on the map to see if there's a change. Similarly, in bowel cancer screening, when you turn 50, you get a pack and then you can test your stool with that pack to check and see if there's any blood that's shed by tumours.
Chris - When I went to medical school, one of the documents that was given to us as students said that a healthy person is someone who's been inadequately screened. I don't know where that fits into the framework you just mentioned, but when we do this, what's the purpose of doing it? Is it just to pick up disease early?
Gerald - If you can pick up something small before it becomes something big, then you can treat something and you have a much better chance of survival as well. Again, in my main field of breast cancer, if you can catch something before it's the size of a 10p, so less than 15 millimetres, with the current treatments and the advances in all the medications that we can use nowadays, you have a 95% chance of survival. If a cancer is presenting much later, that means it's grown into size or is starting to invade the tissue and spread elsewhere in your body, your chances of surviving are less. Likely, you might need more extensive surgery, you might need more chemotherapy or more radiotherapy.
Chris - Some cynics, though, say that when we aggressively screen for things, what we do is turn healthy people into people with a label of disease and they just live with the disease for longer, but they die at the same point they would've done?
Gerald - Depends on the age you are as well as the type of disease that you have. You could be diagnosed with a very slow growing breast cancer, as an example, that would take maybe 10 years before it even doubles in size or spreads anywhere else. This is something called the overdiagnosis debate where you could be labelled with cancer, you have to pay more insurance, you may have problems with travel, but this is the thing that probably won't kill you in the end. You might then die instead of heart disease or something else. Whereas, on the other side, you can have the aggressive cancers and if you catch them earlier, before they spread, then you will have a very long and full life. So that's the balance of screening that we want to do to increase our ability to pick up the cancers that matter and not the ones that will not harm you in the long run.
Chris - We've only got a limited number of screening programmes for disease at the moment though, haven't we? We've got, for instance, breast cancer cervical screening, there's no prostate cancer screening for what is ostensibly the most common cancer in men and a killer of many men. So why are there some things which are screened for but not others?
Gerald - I think that comes down to the accuracy of the screening test. So, for bowel cancer, where they have the Faecal Occult Blood Test, that's shown to have a very high level sensitivity. You have confidence that when you're calling back you have a good chance of seeing a tumour or lesion. The same with breast cancer screening: you'd have to screen a thousand people to find 6-8 cancers and, as such, you need a test that's quite good. Mammography is about 90 to 95% effective. Cervical cancer screening, and diabetic screening is another example, these are tests that have a high sensitivity and specificity. For prostate cancer, at the moment, the PSA, which is the biochemical blood test that's used, they can be inaccurate. As a result you may do more harm than good in having unnecessary surgery, unnecessary worry or biopsies. The UK National Screening Committee is the coordinating body that evaluates screening programmes. They look at all the evidence and say, 'This can now be a national screening programme. There's enough evidence here that this test is the right test and it can find as many conditions as possible.'
Chris - Presumably this is a moving thing in the sense that as new technologies emerge and new practice emerges, it enables us to do it better and therefore what might have been regarded as impractical before is now regarded as a reasonable target.
Gerald - That's correct, yes. I think there's now trials looking at low dose CT for lung cancer screening. You do a health economics analysis to see if the costs of it justifies providing a screening programme. Similarly, with cervical cancer screening, when the evidence of the HPV vaccine came in, that provided evidence of how you balance the screening programmes. So those are the ranges of criteria that you're dealing with: what we can afford to provide and the benefit to the population as well.
Chris - And artificial intelligence - one of the words of the year over the last 12 months and is barely off the front page - that also has cropped up in association with us becoming better and more agile at managing cancer. A lot of times I've noticed.
Gerald - Yes, and it's taking the world by storm. So I've worked with the previous technology, which is Computer Aided Detection (CAD), and what it does is it shows circles around areas that are of worry. With CAD, you could have up to 20 or 30 circles on an image, and that's not really very useful because that's pretty much the whole image covered by circles everywhere. But the artificial intelligence programmes are trained on hundreds and thousands or millions of images and it says, this is what cancer looks like, this is what cancer doesn't look like. Radiologists are the doctors who look at the mammograms, who look at CT scans. There's going to be a 30% decrease in the workforce in the next few years. The Covid catch up, where we had to catch up with all these cases, and the increase in activity and work in hospitals means that the medical workforce is under increasing pressure. In screening, you're looking at a lot of normal cases to find the few abnormal cases, so you could actually use AI to automate the normal cases. We project from the study that we did called Gemini in Aberdeen that you could automate probably about 30% of normal mammogram reading. So instead of 20,000 mammograms a year, I'd be reading 15,000 mammograms a year, and that extra 5,000 mammograms I wouldn't have to read would then free us up to do the harder cases or the more complex mammograms to try and find the cancers in this small group.
21:32 - Immunotherapy: The next step in fighting cancer
Immunotherapy: The next step in fighting cancer
John Maher, King's College London
We have explored who is getting cancer, and of what, and we’ve learned about the mechanisms of the disease and how we can use that understanding to develop better ways to screen and pick up cancer early. We can also use that knowledge to optimally treat the disease. Generally, this begins with surgery to remove the primary tumour where the cancer originated. We may then use radiation to kill off cancerous cells that might multiply very quickly, and chemotherapy - toxic drugs - to target malignant cells that may have escaped.
But some of these treatments can come with very severe side effects. By their nature, cancer cells are relatively similar to healthy cells, so drugs designed to take them out often cause collateral damage. So scientists are trying to work around this problem.
John Maher is a consultant immunologist at King’s College, London. He is also the chief scientific officer at Leucid Bio, a biotech company that develops next-generation cell therapies for hard-to-treat cancers…
John - We target general properties of cancer cells, such as the fact that they tend to grow fast. But the problem with that traditional approach is that other cells in our body also have a tendency to grow fast, such as blood cells, for example, and cells in the intestine. These more traditional, blunderbuss type approaches tend to have a lot of side effects. The way we're beginning to look is to achieve more targeted drug therapies, which hit molecules that are different in cancer cells compared to healthy cells.
Chris - Is that because the cancer cells are effectively afflicted by a genetic disease: cancer is caused by changes to DNA and that makes the cells look different so there are therefore things we can pick on. We can identify those things and go after them because they single out the cancer as different from the rest of the body.
John - Yes, that's exactly right. Cancer cells have been described as being like mutation factories where, as the disease progresses, you acquire more and more of these mutations and it's a bit like a Charles Darwin type process where you get the selection of the fittest cancer cells tending to grow out. But that, in a certain sense, is an achilles heel of cancer as a disease because the more it mutates, the more it makes itself different from a normal cell and the more opportunities that gives you from a treatment perspective to design drugs which can tell the difference between what is normal and what is malignant.
Chris - So how are cancer doctors and scientists trying to exploit those differences? How are you pursuing this?
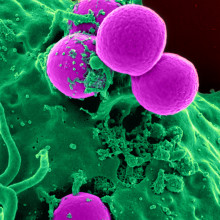
John - Certain genetic abnormalities that are common in cancer can be targeted using drugs which specifically hit that property of the cancer cell. These are so-called targeted therapies. There are pills which can block those abnormal proteins and slow the cancer down. That's one type of approach which people are developing. But the area which I think has really exploded onto the map in this century has been immunotherapy. What that means is actually harnessing the patient's immune system so that it can attack the cancer. Immunotherapy as an approach is as old as the hills. It's been over a hundred years in development and, until about 20 odd years ago, it was considered to be an absolute disaster zone in terms of being completely ineffective. But that mindset has changed radically.
Chris - How do they actually work?
John - So I think we're all familiar with the idea of an antibody as being a protein which can bind onto something. Traditionally what people have done is made antibodies, as a drug, which can bind onto cancer cells and that makes a lot of sense and it can be effective in some cases. But more recently what people have done is to make antibodies which don't actually directly attack the cancer, but instead take the brakes off immune cells. So your immune system is constantly sniffing around the body, looking for things that look a little bit abnormal. But there are a lot of checks and balances involved in how the immune system is controlled. If you can, as it were, disable the brakes of the immune system, you can enable immune white blood cells to see cancer cells more effectively. This kind of approach can be very effective in certain cancer types, particularly a skin cancer called melanoma, for example.
Chris - Does that also have the advantage that, because cancer is growing so fast, there's a chance that it will become resistant to drugs just by bypassing whatever blockade we put in its way by evolving round the problem. If on the other hand you are just unleashing the immune system, it's much harder for the cancer to evolve around that?
John - Yes, that's exactly right. These targeted drugs that I referred to a few moments ago, they will typically go after a single abnormal target in the cancer. Because cancers are mutation factories, what they simply need to do to fly under the radar of that treatment approach is to make another mutation which removes the target of the drug. But when you develop an immune therapy approach such as an antibody that takes the brakes off the immune system, you may have many different immune white blood cells seeing different abnormalities in the cancer. These abnormalities, to use a jargon phrase, we call them antigens, these are essentially things which look different in a cancer cell compared to a normal cell. If you can envisage that you have an army of white blood cells which can each individually see a variety of differences in the cancer cell, it makes it much harder for the cancer cell to mutate its way such that it can avoid this entire army of the immune system.
Chris - I thought, though, that one of the aspects that makes cancer such a malignant disease is that it manipulates our immune system and it even does so through manipulating healthy cells to turn off the immune system or, as you said, fly under the radar. So will this still work if you've got cancer cells effectively hiding from your immune system? Won't they just become better at doing that?
John - That's absolutely right. That goes back to the point that I made about the fact that there are many checks and balances in terms of how the immune system actually works: a very complicated series of molecules, proteins, some of which are designed to turn on the immune system and some of which are designed to turn it off. It's that balance that is critical. You're right in saying that cancer tends to exploit that to increase the negative signals that tend to make the immune system quiet as it were, but these treatments are about disabling brakes on the immune system which will render these immune cells more twitchy, as it were, more likely to attack the tumour. There's a bit of a price that you can pay for that sometimes. That price is that this twitchy immune system can also cause diseases known as autoimmune diseases where the immune system actually attacks your own body. Colitis, for example, where the bowel becomes inflamed, or diabetes where cells in the pancreas that produce insulin are attacked and no longer function.
Chris - Could we go a step further, though, and probe the cancer and say, there are certain molecules that this makes that make it look a bit different and so I'm going to engineer an immune response. So rather than rely on just the twitch of the immune system, actually probe the immune system: this is the target I want you to go after.
John - Yeah, absolutely. So there are two approaches that I'd like to comment on briefly in response to that point. Actually, the first of these is again a very old approach: the development of cancer vaccines. What people are doing nowadays, for example, is you can precisely map out the molecules that are abnormal in the cancer cell compared to the healthy cells. These abnormalities can be used to develop personalised vaccines whereby you inject the patient with something which stimulates immune cells that can naturally see those abnormalities. This is an approach which is beginning to achieve impact in patients at the moment. The second approach that I would comment on, and this is something that I spend my time engaged in quite a lot, involves actually engineering white blood cells of the immune system so that they can detect abnormalities on the surface of cancer cells. Immune white blood cells normally see these abnormalities, these antigens as I referred to them earlier, using a protein which is called a receptor. But what you can do in the lab is design your own receptor, which can enable a very large number of immune cells to recognise a particular abnormality on a cancer cell. This is an approach which is referred to in jargon terms as CAR T-cell immunotherapy. This approach has been dramatically effective in the treatment of patients with selected blood cancers: leukemias, for example. These are patients who have otherwise untreatable disease who, when they are treated with their own genetically modified CAR T-cells, up to 90% of these patients can achieve a complete remission of their disease. These are just two examples of how we are using a variety of engineering strategies to reprogramme the immune system against cancer.










Comments
Add a comment