The recent invention of powerful precision tools for editing the human genome - known as CRISPR, has opened up new worlds of possibilities for researchers seeking to understand how our genes work - and also those who want to permanently change the human genome for generations to come. But are we on the road to designer babies? Plus, we unpack the latest cancer breakthrough, and our gene of the month is making a terrible racket.
In this episode
01:16 - Nick Peel - CRISPR and cancer
Nick Peel - CRISPR and cancer
with Nick Peel, Cancer Research UK
Kat - In last month's podcast we took a look at exciting new technology for altering genes, known as CRISPR/Cas9 - or CRISPR for short. In just a couple of years, these tools have revolutionised the world of genetics, raising the possibility of treating illnesses caused by faulty genes, or even genetically engineering designer humans. That's something we'll return to a bit later, but first I wanted to find out more about how laboratory researchers are using CRISPR to delve into the secrets within our genome. To get the low-down I spoke to Nick Peel from Cancer Research UK.
Nick - Scientists have been working with cells that they grow in the lab and they've been tinkering with genes in a bit of a slightly inefficient way and a haphazard way, kind of inserting bits of genetic material into the cells that might target a gene and switch it off. But the efficiency is a bit hit and miss and they're also sometimes not very accurate in the genes that they see cow and kind of untangling the effects of that makes it quite confusing for the scientists and searching for better methods to piece that together is what they've been after.
Kat - These new and more precision techniques, where do they come from and why are they better?
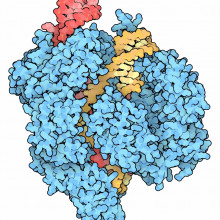
Nick - So kind of a newer invention being using proteins to guide the changes that you might be making to DNA a bit more precisely. So, bringing along with it a certain type of enzyme that's going to cut DNA in a place that you know for sure is where you want that cut to be made or that change to be made. It brings with it greater efficiency and more precision. But the problem that scientists have come across with some of these technologies is they're really expensive and also really time consuming.
Kat - And now, we have CRISPR which, I've heard, best described as sort of a molecular satnav, a very small fragment that guides these molecular scissors to DNA, can cut, can then paste things exactly where you want them with much higher efficiency. How has this changed the game for researchers studying genetics?
Nick - The researchers I have spoken to has basically changed everything for them. It's opening up questions that they never thought were possible before. They're more precise, they're efficient, they cheaper, and an extra thing - they're easier to do. So basically, you can teach anyone how to use CRISPR in a week basically and that's very exciting for researchers.
Kat - How are researchers using these molecular scissors to start unpick what some of these genes do?
Nick - The exciting thing about CRISPR is that you can go as big or as small as you want. So, you can talk of those 3 billion letters and the beauty of the technology is that if you imagine - I've heard it described as imagining the genome like an encyclopaedia - this technology allows you to pick out a volume, open a page, go to a particular page, pick out a word, find a letter in that word, and change the spelling. That sort of precision is just something that researchers have never had access to before and that's why they're so excited about it. And then out of that, you can make those single changes in spelling within DNA and look what that does to cells or whole organisms. But you can either chop out whole genes, rearrange them, tag things onto them so you can see where those cells are, what proteins are doing within cells. It's quite an exciting array of opportunities.
Kat - It is incredible that this really feels like a tool we can use to understand what's all the dark matter of the genome because so little of our genome is the actual genes, the actual things that are the instructions for proteins. All the rest is like... stuff that does something.
Nick - Yeah. The stuff that maybe does something and waving arms around. We need to know what that is and what this technology can do is, as you say, kind of pick into some of those darker regions. You can make these edits to a cell's own DNA. Classically, researchers relying on making a chunk of DNA, sticking into a cell and hoping that the proteins that come out of it that are made of, who knows what amount within the cell, might tell you something. Instead here with CRISPR, you can actually go in and directly change that cell's DNA and look at any bit that you wish and see what happens.
Kat - You work for Cancer Research UK. What are the ways that Cancer Research is using this? Is it going to be a cure for cancer? Can we edit out cancer genes or is it a bit more subtle than that?
Nick - The idea of editing out those kind of faults in DNA that might lead to cancer is an exciting possibility but one that's a lot further away from what the scientists are currently using CRISPR for. What they are doing is taking things like, we know a particular gene fault increases the risk of a certain type of cancer, say. But we don't really know what it's doing, why it might be having that effect. So, what we can do now is start to edit in those precise faults that you do see in people's own genomes, in patient's genomes and really start to see what effect that's having on those cells and build a clearer picture. If that then one day becomes something you can do in people is a much further away discussion.
Kat - I guess it's also very useful for building models of cancer. We've seen in the past few years how we've gone from having cancer cells grown in the lab to bits of tumours transplanted into animals to actually making genetically engineered mice that carry the faults that lead them to develop cancers. I suppose CRISPR is revolutionary here in that you can precision engineer those faults rather than going through the long and tedious process of traditional genetic engineering in mice.
Nick - Absolutely. One of the problems with the older techniques was that scientists were spending years and years, and years, only ever kind of getting to the top level understanding of what one gene might be doing. You can now engineer in multiple different faults in different genes. We know that cancer is a really complicated disease where it's a whole constellation of genetic changes that are going to be behind that disease. You can now start to piece that picture together inside a mouse or a cell or relevant kind of model and get a much better understanding of how the disease works. In terms of kind of working with those models, we know that not only that but being more efficient and more precise in the work that it's doing means that those researchers can work more quickly, more efficiently, and just do a better job all round basically.
Kat - Nick Peel from Cancer Research UK, and I recommend reading the post about CRISPR that he's written for the charity's blog - you can find the link from this podcast's page at nakedscientists.com/genetics
http://scienceblog.cancerresearchuk.org/2016/02/01/crispr-gene-editing-n...

07:39 - Tony Perry - Engineering humans
Tony Perry - Engineering humans
with Tony Perry, University of Bath
Kat - It's time to hear again from one of last month's guests - Professor Tony Perry from the University of Bath, who I spoke to at a conference on human genome editing organised by the Progress Educational Trust. Following on from our previous conversation about some of the ways scientists are hoping to use CRISPR to treat diseases within the body, I wanted to find out how the technology might be used to engineer humans free from genetic conditions, such as cystic fibrosis, which is caused by inheriting two faulty copies of the CFTR gene. And just because we can - does that mean that we should?
Tony - Using CRISPR/Cas9, we could edit a one-cell embryo so that its genome doesn't any longer have that deletion. It has what everybody else has. Because we make the edit in a one-cell embryo, when the one-cell embryo divides, the genomes of those two cells will also inherit the edit that we've made. When they divide, and so on and so forth, so that when the child is born, all of the cells in the child will now contain the repaired version of the cystic fibrosis gene, so they won't get cystic fibrosis. So the reason is very useful, is that we could - or potentially, this is what excites people is that we can have anticipated this disease by repairing the predisposing genetic change that causes it.
So people are obviously very excited by that, not just because of cystic fibrosis although that's very important, but because there are many other conditions. And so, cystic fibrosis as an example of what's called a monogenic disorder where it's thought that a single gene can give rise to the condition. It's thought that between perhaps 3,000 and 5,000 of these conditions exists - up to 6,000. And so, although individually, they're extremely rare many of them, collectively, they really add up to something, hundreds of thousands or millions even in the UK.
Kat - Those are conditions that seem to be linked to one particular gene fault, but the more we learn about diseases like diabetes, heart disease, the common things that tend to plague us, it seems from the genetic research that it's due to lots and lots of gene, or lots of more subtle variations and certainly, many types of cancer as well. There aren't many like the cancers that are linked to specific faults in the BRCA genes like breast and ovarian cancers. How can we possibly go in and tinker with all of those variations? How is that going to work for these more common diseases that are linked to lots and lots of gene faults?
Tony - Well, these are very good questions and so, we don't know. But certainly at the moment, there is every prospect that yes, we will be able to go one day in the future and edit the predisposing alleles for multiple genes. At the moment, the record is 62 in one swing of the bat. And so, it may be more and there are going to be issues and life is never that simple is it? But what we have to remember in all of these I think is that there are two things. One is that the CRISPR/Cas9 technology is not the only technology. There's DNA sequencing technology which is also marching ahead of the furious pace and which will feed into this discussion. But the second thing is that the CRISPR technology was first applied and reported in February 2013. So, this is fewer than 3 years ago. It's remarkably soon after that first report in mammalian cells of CRISPR/Cas9. And already, we're talking about these incredibly ambitious goals. So, I think if it continues to make the progress that its made so far, we should have every hope that CRISPR/Cas9 technology will be made safe enough for multiple human applications if we decide to apply it in that way.
Kat - What are some of the questions that people have raised about the safety, the accuracy of this kind of technology when it comes to editing humans?
Tony - Well, I think you raised a good point and it's clearly a major bug bear. What is the specificity of this system? So, we have a system that's highly accurate, but from time to time, it makes a cut where we don't intend it to make a cut. So, we can now use whole genome sequencing to find out or learn more about that off-target cutting. And that means that we can design, we can engineer improved scissors, improved satnav so that the off-target cutting becomes less and less frequent. This is already very soon after that first since the advent really of CRISPR/Cas9 in mammalian cells. So, I think that we should be very optimistic that we can - scientists, scientific community can present the rest of society with the tools that are safe enough for these human applications, should they decide to use them.
Kat - It seems fairly obvious to me that there's going to be a point where we can do this and the big question is, should we do this? How is that discussion playing out, not just here in the UK, but around the world?
Tony - It's interesting. The main centres of the discussion that I'm aware of are of course in the US where most of the technological advances have been made. They've done a fantastic job there and in the UK, where there's been a great deal of discussion about this. There's also, we shouldn't forget China where the only report so far to be published of a human embryo genome editing using CRISPR/Cas9 appeared in April 2015, this year. So, these are the main places. The dichotomy really seems to be between people who say, we should at least explore the possibility of using this for medical applications. By this, I mean the CRISPR/Cas9 editing, and those who say, "No, just no. It's crossing a line" and that's the phrase that Francis Collins, the director of the National Institute of Health in the US used at the end of April in 2015 when he came out and made a statement as a director. He and others think this is just crossing a line which is never justifiable and the line is one where are now doing as you suggested, we are editing the human genetic contribution to our makeup and that's something we just don't get to do.
My view is that actually, these considerations must be heard and respected - all of them - those pro and those anti. At this stage, because the discussion, although it's raging at the moment and I'm glad it is, it's still quite young. It will be altered as technological advances get rolled out and continue to come at us - as I said that they're not just in the editing but also in the whole genome sequencing field. We shouldn't rush to conclusions. So, my hope at the moment is that the discussion is as informed as possible about the science of what's going on rather than being utterly speculative and based on things which are a little bit sometimes fanciful.
Kat - We've talked about using this kind of technology for curing or preventing the development of diseases, but what about say, I have a friend who has a yearning to have a fish's tail or something like that or maybe if I wanted super senses or something like that? Are people interested in editing maybe non-human characteristics into ourselves or enhanced human characteristics?
Tony - This is very interesting and it's really in the realms of speculation. But yes, certainly, people are interested whether it be - maybe not so much although I don't know people who want to become or for their children to be like mermaids - but certainly, yeah, combat troops of the next generation who have infrared vision for example or can smell certain odorants that other people can't detect. These are the kind of things that the kind of applications that some people might consider, and there are many, many others and it's quite good fun - I don't want to trivialise it - but to make lists of these things, the attributes that aren't directly disease-related but you might introduce it into the human germline.
The thing about this and that the problem with this is that it's not really in my view an issue particularly for the editing technology. Once we have the tools for the editing and the vision for what we want to do, we still have to know how to apply these tools to get to that vision. This is what I call process. Unless we have the process right, we'll never get to the vision. By process in this case, I mean, what genes are you going to edit and exactly how? Maybe which regions of the genes? So, you could take a very simple one. I don't know if it's important but it's simple to describe because - and you did so of adding a fish's tail onto a person so that they're like a mermaid perhaps or merman. Well, just where do you start? We're nowhere near knowing how you would do that. In terms of the Hox gene expression, this is the days of the segmentation gene, the Homeobox gene transcription factors that control limb development. We're just in the tall grass, still in the basic biology.
And people talk about IQ. I want my kids have an IQ of 300. Well okay, tell us which genes to edit and we'll see what we can do. We just have no idea at the moment for many of these things. And so, a lot of this talk of these extra traits is utterly fanciful. It really belongs to the realms of genetics. It doesn't have all that much to do with CRISPR/Cas9 per se, even if that's your vision. And until people can tell you, "Look, we have now a very good idea that this gene, this gene, this gene, expressed at these different levels" and there might be hundreds different splice variants, different variants of the genes at different levels at certain combinations might give you an IQ of this." Then we might think about, "Well, do we want to do that and how we want to do that using the CRISPR/Cas9 technology?" but for most of these, we're nowhere near getting there.
Kat - Tony Perry from the University of Bath.
19:21 - Alan Worsley - Targeting cancer
Alan Worsley - Targeting cancer
with Alan Worsley, Cancer Research UK
Kat - It's time to take a closer look at one of the biggest cancer stories to come out in the past month, grabbing headlines such as "A cancer cure in just one jab?", "Scientists find cancer's Achilles' heel", and "Scientists claim cure for cancer is closer". So is it? And what's the science behind the headlines? I spoke to Alan Worsley, senior science information officer at Cancer Research UK - who funded the work - to get the background to the story, and what it all means.
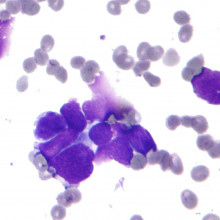
Alan - One of the researchers, Professor Charlie Swanton who works now at the Francis Crick Institute, for the last few years, he's been really trying to look at how the genetic landscape of a tumour is shaped. So what this means and he's particularly been interested in how there are differences in mutations across the tumour. How does a tumour begins, starts off? And how certain mutations has got it to that point, has got the cells growing more quickly? But as the tumour grows, different sections will take on their own mutations, particularly if the cancer has developed in such a way to make more and more of these mutations happen. This is what they call "tumour heterogeneity" which is a really fancy way for just saying that the tumour looks very different depending on what part of the tumour you look at.
Kat - I like the idea that it's a bit like a patchwork blanket - that it's made up of all these different bits that are related but kind of look different.
Alan - Exactly. The reason he's been looking here, he's long been researching in the cancer such as lung cancer, kidney cancer where they tend to have a lot of these mutations. The tumours do look much more like a quilt, patchwork blanket than other cancers which usually are - there's kind of one or two main mutations driving that growth. The problem is, this patchwork makes it really difficult to use standard chemotherapy and radiotherapy - drugs that do their best to wipe out fast growing cells. Because there's so many mutations, it seems to be easier for these cancers to evolve a way around it, to evolve resistance.
Kat - I guess there's a chance that even if a small pocket of cells is resistant to that treatment then they're just going to carry on growing it and start again.
Alan - Exactly. So that's what we tend to see, that a treatment might seem to work but then the patient relapse and then that pocket of cells has by chance happened to have a mutation that makes them resistant to that particular treatment, they then grow back. So this is what has made these types of cancers so difficult to treat for so long. It's really been kind of one of his goals to try and find a way around this. How do we get past this? So initially, his thoughts were, if we can find treatments that effect what he calls "the trunk". These are the mutations that are right at the beginning that should be present in most of the cancer cells. If we can hit that with drugs and find out which drugs would be best for which patients, we might have a better chance.
Kat - These are these kind of molecularly targeted drugs that we've heard about lately?
Alan - Exactly. So, this is for the past 10 years, where 10 years ago, this was seen as the future of cancer research - targeted therapies, going after precisely the molecular problems that are associated with your individual tumour. Now, the problem is that for every single one of those mutations, you need a different drug. For every single one, you need to find a targeted therapy that suits that patient and they're difficult to make. They're difficult to find the chemicals that will accomplish this.
Kat - And incredibly expensive.
Alan - Exactly. So, it's going to take a lot of work to come up the suite or arsenal of target therapies you would need to hit every tumour.
Kat - And of course, when you start adding drugs together, you've got more side effects, the chance of more toxicity. I've heard people say, "Well, if we could have the right combination, there's no guarantee that it wouldn't harm the patient before it's actually treating their cancer."
Alan - Precisely and that's really been the biggest challenge facing that.
Kat - So, with this new study, what's the twist on it here because that seems almost like an insoluble problem and I've sat through conferences where people go, "I don't know how we're going to make this work." What's this new study all about that actually gives us hope that there could be a way through this problem?
Alan - So, the big difference within the last five years has come the rise of immunotherapy, using the immune system to fight cancer for us. So rather than banging our heads against the wall, trying to find what small chemicals can stop these mutations, the difference is that every one of those mutations and there are hundreds, hundreds of these in every cancer gives a chance for the immune system to recognise that something is wrong. And that was the big revelation.
Kat - Why doesn't the immune system normally just mop up cancer cells because these are kind of rogue cells, they're not right? What goes on that the immune system doesn't go, "Stop! Let's get rid of you. You look dodgy"?
Alan - Well, this is the exact paradigm that's so fundamentally changed in recent years. We used to think, it must be just rubbish at curing cancer. If we had an immune system that could take this out, why are we even getting them? The answer is actually, it's probably wiping out cancer in you all the time. It's actually exceedingly good. In fact, it's the other way around. For any cancer to develop, it has to have found a way to escape the immune system. And that's been the real change that people have realised, if you just find out how to get the immune system to target cancer, you can have really stunning results.
And that's been shown in new drugs that have come in the last few years. These are drugs specifically that take the brakes off the immune system for any established tumour, especially the very tumours that Professor Swanton has been looking at, these highly mutated ones are precisely the ones that actually would be most recognised by the immune system. And for them to exist, they have to have one of a handful of tricks to get past the immune system. And one of the things they found in this research is that precisely, the most mutated tumours are the ones that are most likely to have to have very specific immune evading mechanisms.
Kat - What are the sort of topline experiments that they've done and the key findings that have come out of this?
Alan - So, the main thing they did was that after years and years of trying to track down how mutations are different across cancers, these are specific DNA faults, they said, "Well, what does this mean for the immune system? What is it that the immune system could be recognising that maybe our drugs can't be hitting?" So, they applied the same computational power to look at what's known as antigens. An antigen is any protein that through a DNA fault, looks a bit different than it normally should. Now, every cell on the body, does what's called as antigen presentation. They take a sampling of the stuff they're making inside a cell and hold it out for inspection. It's like factory managers coming in, taking a small sample saying, "Yeah, this looks right. This lot is good to go. This looks funny. No, no, no. Stop the whole line. Something is wrong here." This is known as immune surveillance. They're surveying all these cells to make sure they're doing what they should be doing. So what they found is they used computational power to predict what sort of antigens might be there. Their theory was based on the same thing they're doing with mutational stuff is that, can we find antigens that are present across the entire cancer? Can we find ones that, if the immune system had to recognise something, we want it to be one of this lot.
Kat - And that should be present on every single cancer cell.
Alan - Exactly. This is a whole problem, it's that for some treatments, this is getting back to the whole relapse. If you've got a drug that only targets a portion of the tumour, all you're going to do is leave behind resistant ones that are going to grow back and now, you've got a cancer that's resistant to the treatment you had. So, if we're going to aim this at something, aim it at something that's across the entire tumour. So that's what they did. We didn't know if these things actually existed. We just didn't know until this paper had come out.
What they did is they went into samples they had already analysed, a prior study, and said, "Right. Can we find out whether or not the immune system can find these antigens?" So what they did, ran their analysis, they predicted hundreds of possible antigens and then they essentially fished out, to see if they can find any immune cells that recognise them. And they got three hits in two different patients - 1in one, 2 in the other, and each hit was exactly one of these, what they called a "trunkal antigen", an antigen present across the tumour. So proof of principle, these things are there. If we can find them, then we can either take them out, multiply them in a lab and stick them back in, or use the drugs that release the brakes and help those cells get to where they need to and hopefully, kill the entire tumour.
Kat - This at the moment is research that's been done on samples from a handful of patients. People have got very excited about this, the idea that maybe you could have a personalised immunotherapy - you could take samples from a patient and say, "Okay, this is the kind of things that we need to be targeting." Realistically, how close is this to being a treatment and what are the steps that need to be taken to turn this into a viable treatment?
Alan - So, I think the main thing about this research is that this isn't a new treatment per se. this is a guidance system for treatments that we've already been trying. So even in the news recently, we've heard about scientists taking immune cells out of the body and re-engineering them so that they could target cancer and then putting them back in or just simply taking immune cells that we think recognise a right thing and growing them up in the lab and putting them back in. Or these checkpoint blockers - these are drugs that take the brakes off the immune system. This gives us the guidance that we've been lacking.
At the moment, we've been sort of flying blind. We've been trying these treatments and in a portion of patients, they looked really, really well. But the vast majority don't seem to respond. So this guidance could say, "Right. For these patients where we could see they've already got immune cells that are targeting the best possible target, we didn't need to cut the brakes. The immune system is already locked on. It's just being held back. Those patients, they just need those drugs. For other ones, maybe we could say, "Right. These patients, they've got a lot of possible antigens. There's a lot of distractions for the immune system here, but we know they've got cells that lock into the right target. Maybe those guys need a bit of help and it can help guide what we should be doing."
Kat - That was Alan Worsley from Cancer Research UK, and that research was published in the journal Science.

30:01 - Gene of the Month - Cacophony
Gene of the Month - Cacophony
with Kat Arney
And finally it's time for our noisy Gene of the Month - it's Cacophony. A gene found in fruit flies, Cacophony encodes part of a special tunnel-like protein called an ion channel, found in the nerve cells within the insect's brain. It's responsible for shuttling calcium ions across the borders of nerve cells, which is essential for enabling these cells to send and receive messages correctly. Scientists have found that having a certain faulty version of Cacophony can cause flies to have epilepsy-like seizures. But - strangely - it actually prevents seizures in fruit flies that carry another faulty gene, called paralytic-bss1, which also makes them susceptible to the fly version of epilepsy. And it has the same suppressing effect in flies carrying seizure mutations going by the wonderful names Easily Shocked and Slamdance. But, of course, this is of greater importance than just insects - around one per cent of the population is affected by chronic epileptic seizures. Figuring out the interactions between Cacophony and these other genes is helping to shed light on how ion channels interact in the brains of humans affected by these conditions, paving the way for more effective ways to control them in future.










Comments
Add a comment