This month, we’re peeling back the science of the peripheral nervous system, looking at some of the injuries it can sustain, and taking a closer look at exciting new developments on the horizon for treatment. Plus, we’ll be digging into the latest neuroscience news, with the help of some local experts.
In this episode
00:56 - ADHD, Mind Wandering and Cycling Accidents
ADHD, Mind Wandering and Cycling Accidents
with Duncan Astle, Cambridge University; Helen Keyes, Anglia Ruskin University
Cambridge University cognitive neuroscientist Duncan Astle and perceptual psychologist Helen Keyes from Anglia Ruskin University sifted through the latest neuroscience news, and told Katie Haylor what caught thier eyes...
Duncan - The authors are really interested in attention deficit hyperactivity disorder or A.D.H.D. One of the symptoms of A.D.H.D is increased prevalence of mind wandering among other symptoms but of course we all know that you don’t have to have a diagnosis of A.D.H.D to suffer from mind wandering. It’s something that we all encounter.
They were really interested in understanding the neural mechanisms behind mind wandering and how that might interact with cognitive skills. So they got 185 young adults. They put them in an MRI scan and they made them perform a task called an N-back task. It's a very simple short term memory task and periodically they would stop the task and they had a series of questions about how well concentrated the individuals were, what they were thinking about, how hard they were working on the task, what their minds were on. They had quite detailed information about mind wandering and these were interspersed throughout the task. And at the end of the scanning session they also rated the subjects for their A.D.H.D like symptoms.
And what they found really interestingly was that those who had high ratings of these symptoms firstly they would be more likely to mind wander. That tells us that indeed it is the case that these things vary naturally throughout the population even in people who don’t have a diagnosis, and they found that those people who did mind wander more, they performed more poorly on visual memory task on the N-back task and then when they looked at the neuro-imaging data they found that areas of the brain involved in what we call cognitive control so areas in the frontal lobe and areas in the parietal lobe, the connectivity between these areas and sensory areas like visual cortex would drop out periodically. And in those moments, subjects are more likely to mind wander and that's when their cognitive performance would drop.
It's a really nice demonstration of how you can link these sort of higher order symptoms that we all encounter and that are very common in kids with A.D.H.D. Linking it to a neural mechanism, and then there's a cognitive outcome which in this case is visual short term memory.
Katie - What would you recommend somebody would take away from this study?
Duncan - Firstly is to say the mind wandering that we experience as a sort of a very higher order phenomena that happens all the time, actually has some really basic underlying neurobiology to it that we're starting to understand. Secondly that it happens to lots of people. And thirdly that it happens to some people an awful lot and that's because this neuro biological mechanism is more likely to kick in in those individuals.
Katie - Helen, any comments?
Helen - Yes so you said they noticed a correlation between instances of mind wandering and the dropping of the connection in the brain areas. So which drove which?
Duncan - It’s very hard to say. The way that I would think about it is that it's one process that we can analyse at two different levels so we can analyse it at the kind of experiential level that describes the experience of switching off and the zoning out. And then at the same time there's underlying neural correlate can be demonstrated. Now those two things go hand in hand. There may be some previous mechanism that causes both but I think these things are just sort of two halves of the same coin.
Katie - Thank you very much. So Helen you've been looking into a paper about whether or not we should be wearing helmets. Particularly pertinent for people who live in Cambridge these are cycling helmets. What were this group trying to find out?
Helen - They were trying to find out whether wearing a helmet would make you take slightly more risks and they were measuring this by looking at how you perceived distance between you and threatening objects or you and non-threatening objects.
Katie - What were these threatening and non-threatening objects?
Helen - So in a very realistic setting, they used pictures of a tiger or shark as you would commonly encounter in Cambridge! That was the threatening stimuli, or non threatening stimuli such as rabbits, mice, horses, things like that.
Katie - OK. So this is a lab study trying to replicate behavior perception when you wear a helmet compared to when you don’t when you’re cycling. What did they find?
Helen - So they found that if you wear a helmet compared to if you wear a baseball cap, you did risk compensate. So for objects that you perceived to be non-threatening such as horses and rabbits, you actually overestimated the distance between you and them, you thought they were further away which suggests wearing a helmet made you feel safer, you risk compensated.
Some good news for helmet wearers is that this didn't apply for threatening objects, so when there was a threatening stimulus in front of you you re-adjusted your risk level, it overrode that risk compensation behaviour and you saw the threatening object as close to you. Similar to people in baseball caps. So people in baseball caps saw threatening and non-threatening objects as quite close to them. People with helmets saw threatening objects as close but safer objects as further away, they overestimated that distance.
Katie - So what should people take away from this with regard to their cycling behaviour? Because I certainly would always wear a helmet!
Helen - So it does add to the debate in an interesting way because it suggests that wearing a helmet can be positive. The general worry in wearing a helmet is that we recalculate the level of risk, feeling safer and therefore we take more risks. So this study is saying, actually, if a threatening situation arises you will suddenly recalculate your risk taking into account that threat and you will perceive things safely. So the presence of a threat will override that overconfidence is what this paper is saying.
However it also suggests that if you’re not expecting a threat, so if you’re cycling along feeling quite safe, you will be a little bit cocky and take those risky behaviours. So they’re saying you overestimate distance, you take more risks if you feel quite safe as a cyclist wearing a helmet. Whereas you don’t do that when you’re not wearing a helmet.
So you can take from that what you will. On the one hand it's comforting to know if you wear a helmet you will recalculate your risk perception if a threat is present but if you don’t perceive that threat you could be engaging in risk taking behaviours that you wouldn't otherwise engage in.
Katie - Generally, how much evidence is there to suggest wearing a helmet can put us at risk?
Helen - There is quite a lot of evidence coming from road cyclists and drivers. So we know that drivers will give cyclists less space when they're overtaking, if the cyclist is wearing a helmet and we know from numerous studies that cyclists engage in much more aggressive cycling much more risk taking behaviour when they're wearing a helmet compared to when they're not.
Katie - But is it also fair to say that we do know a cycle helmet can make a vital difference if you are involved in a crash?
Helen - If you are in a collision, without a doubt, you need to be wearing your helmet. Your wearing a helmet is going to significantly reduce the chance of brain injury. The same is also true though for pedestrians and car drivers, so if you are a pedestrian perhaps you should also be wearing a helmet. And interestingly on a numbers level, if you are in a car accident let's say you're a driver compared to a cyclist. If you're both in a collision, the cyclist is going to need the helmet more than you. But on a pure numbers level the amount of people that are in car collisions every year. If all drivers mandatorily wore helmets we would decrease the level of brain injury more than if we ask cyclists to wear helmets, because it's just fewer cyclists and we would probably think it would be a bit mad to start saying drivers should wear helmets.
Katie - Duncan, do you cycle around Cambridge?
Duncan - I do, and I do wear my helmet. I'd like to think I am reasonably cautious with my helmet on. I guess it's one of those things were there are probably massive individual differences. There are some people who presumably are such cautious cyclists they'll be cautious regardless of whether they wore a helmet. Whereas there are presumably some people who share a big helmet effect and cycle very differently.
Helen - I do insist that my children wear helmets, so I'm a bit of a hypocrite.

10:12 - Temperature and touch
Temperature and touch
with Adam Murphy, Hannah Laeverenz Schlogelhofer
What exactly does the peripheral nervous system do? Katie Haylor recruited a few unsuspecting colleagues to find out. First up, Katie challenged intern Hannah to, solely by touch, pick out a two pence piece from a pocket full of different coins...
Hannah - This first one feels quite smooth, a bit too small for 2p to think it's a 1p.
2p is one of the larger ones I think I'm gonna go for this one…. No!
Katie - So you picked out the 50p. How come?
Hannah - It felt like it was the right one, but no….
Katie - Harder than it sounds, right? Now Hannah was integrating temperature differences, size and shape differences, whether they were ridges on the coins and so forth, all in order to help her make that admittedly wrong decision. So what are Hannah’s peripheral nerves actually doing?
Well sensory nerve endings stretch out into the skin and there are different types of receptors on the end ones that respond to temperature, pain and pressure. For instance when Hannah feels for example the ridges on a five pence piece compared to no ridges on a 1 pence piece, those signals rocket up the nerve cables called axons to the sign ups where chemicals move across the gap and the electrical signal continues on to other nerve cells up to the brain, where that information is interpreted. But just how good is the neural resolution in our peripheral nervous system? Time for another test. And this time it’s on Adam.
Katie - I'm going to touch your finger and I want you to tell me how many different points are touching you - ready?
Adam - That was one, and that felt like one too. That was two.
Katie - Okay now I’m going to do the same thing on your leg. Ready? Yeah.
Adam - One, one and one too.
Katie - Hmm. Well he got it right for the finger touch but completely wrong on the leg. I was using a pen and a pencil. So two points of contact every time and they weren't even that close together. So what's going on? Well nerves are concentrated differently in different areas of the body. Fingertips or lips for instance have lots of nerve endings and therefore a much higher resolution than say the back of the leg. And this makes sense from an evolutionary point of view as you don’t routinely use the back of your leg to pick berries from a bush or to kiss your loved ones.
Time to terrorize my colleagues a little more. Some aspects of the peripheral nervous system can be tricked. Let's take temperature for instance. Now have you ever wondered why chilli tastes hot? In order to see how well Adam and Hannah could discriminate spicy food from hot food, I challenged them to, with eyes shut, taste and identify microwaved pieces of red pepper against pieces of room temperature, but seriously spicy, chilli pepper.
Katie - Pick up the fork. There we go.
Hannah - Where is it!?.....
Katie - Hannah’s doing pretty well, Adam, you’re doing badly… OK you've both got some, now have a taste. Is this red pepper or chilli pepper?
Hannah - I would say the regular pepper.
Adam - Yeah I'd agree, that one doesn't feel particularly spicy.
Katie - OK, next try the other one….what do you think?
Adam - Well my face hurts now, so that’s spicy!
Katie - I'm not sure Adam will be going near a vindaloo any time soon. So I failed to fool them but it seems like the chilli didn't. Spicy food like chilli contains a chemical which binds to a receptor responsible for detecting temperature, in this case high temperatures. So activating this receptor causes our bodies to interpret chillies as being hot, when really they're not at all. But knowing that won't stop me from downing water or better still milk after taking on a particularly serious curry. So that's hot. What about cold? Well it seems a crafty chemical called menthol is also rather good at this molecular trickery. Menthol - you guessed it - can also bind to a receptor normally responsible for detecting temperature. In this case the cold. And this is why menthol-containing mints can make your mouth feel cool.
Hannah - If you just chew it, doesn't feel cold but when you breathe in, you get like a cold breeze coming in so it feels like a gust of wind in your mouth. It's like a whole storm happening in your mouth like a cold air.
Katie - And how does this compare to ice chips because they're genuinely cold? So if you can fish around in that bucket, there should be some ice and there's a tiny little ice chip. Adam's going for it, off we go...
Adam - Really cold!
Hannah - It’s more all-encompassing cold!

17:37 - Peripheral nerve injuries
Peripheral nerve injuries
with Rhys Roberts, Cambridge University and Addenbrooke's Hospital
Peripheral nerves put up with a lot, but sometimes things do go wrong. To find out how peripheral nerves can be damaged, Katie Haylor spoke with consultant neurologist and researcher Rhys Roberts from Cambridge University and Addenbrooke's Hospital...
Rhys - Diseases of the peripheral nervous system are generally called peripheral neuropathies. There are various estimates but roughly around 2 percent of people will have a peripheral neuropathy at any one time and some estimate that as we get older it can go up to around 8 percent of the population. Now peripheral neuropathies themselves, the problems can be split into two main types. So there are conditions that you have inherited, these are genetic conditions many of which as we now are able to sequence DNA much easier than previously, we’re able to pinpoint specific changes that lead to diseases of the peripheral nervous system, but also a very large group which are what we call acquired so these are factors which have come in from outside.
So within the acquired part there's a very very very long list of other conditions that can lead to peripheral neuropathies and these can be other medical conditions or they can be certain things that have affected the nervous system, either being exposed to an agent or a medication that has been used for another condition which has had an effect on the nerves.
By far the commonest cause of peripheral neuropathy that we see is due to secondary related diabetes. So roughly two thirds of people with both Type 1 diabetes and Type 2 diabetes which you've heard of will have a neuropathy. So this is very common and if you think how common diabetes is, and the commoner it gets with time this is a significant problem. Clearly to what extent people living with diabetes will be affected obviously varies from person to person, and also how well controlled the underlying condition is. Of course people with diabetes can often have an affected autonomic nervous system as well which can have an effect on their blood pressure and their ability to sweat and also on their gastrointestinal system.
Katie - So why would diabetes cause nerve issues? Because you do hear about people having tingly feet or tingly fingers, why is this the case?
Rhys - That's a very good question. We don’t quite understand why diabetes affects the nerves. What we do know is that the nerves are supplied by very small blood vessels. And plays a very important part in the function of the peripheral nerves. We know in diabetes that the blood vessels can be affected and there's certainly a higher risk of cardiovascular disease so it is likely there’s going to be a combination between the high sugar, the dysregulation in fats, and also the effect on the smaller blood supply certainly to the longest nerves.
There’s trauma. So when people have injuries and so forth that can sever the axon of the peripheral nervous system meaning that the signals can’t get across that injury and anything downstream of that site will either be weak or you’ll be numb.
Katie - So this is a physical trauma that essentially snips apart, almost like a pair of scissors, the nerve and it becomes disconnected?
Rhys - Correct and whilst the nervous system and the Schwann cells in particular will react to these injuries in an attempt to guide the growing axon back to where it was before, this not only can take a long time but on occasions the axons won’t get back to exactly where they were previously.
Katie - So can that result in paralysis then?
Rhys - Yes yes. So any structure that was innovated then by these nerves essentially the signals wouldn’t be getting to for example the muscles. So you’d be weak, the muscles will get smaller. Leading to the inability to move or perform a function, and likewise any signals that came back by that nerve to the spinal cord to convey any sensation and so forth and that would be impaired as well.
22:48 - Gels to help nerves re-grow
Gels to help nerves re-grow
with James Phillips, UCL; Rebecca Shipley, UCL
Our nerves are very resilient. They run along limbs where they bend and stretch with our daily movements and conduct the impulses necessary for sensation and movement. But physical trauma is one case in which nerves sometimes simply cannot take the strain. So what can be done to help when nerves get severed? The gold standard currently is a surgery called an autograft, taking healthy nerves from somewhere else on the body, usually the leg and putting them into the damaged site to hopefully regain function. But this means another surgical procedure with all the associated risks, injuring another part of the body, and of course scarring. Nervous system tissue engineer James Phillips and biomechanical engineer Rebecca Shipley together direct the Center for Nerve Engineering at University College London and they've been working on gels which would be implanted at the injury site, encouraging the severed ends of nerves to regrow. They told Katie Haylor about their work...
James - We're trying to learn from the nerve graft approach and to try recreate that in the lab effectively by trying to make an artificial nerve tissue that could be used instead of a nerve graft.
So this would have the same support cells and the extracellular matrix that you find in a nerve graft, but it would be made in a lab so you wouldn't need to go and harvest a bit of healthy tissue from somewhere else on your patient.
Katie - What goes into growing a nerve naturally, and therefore what do you need to put into your artificial tissue to encourage nerves to regrow?
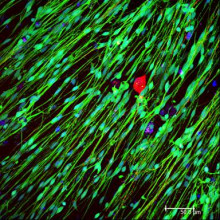
James - Peripheral nerves do have the capacity to regenerate after injury but only in the right environment. Now the right environment is actually the inside of a damaged nerve, so the neurons have died away. What you're left with is just the support cells and the extracellular matrix that used to be there. Those support cells are called Schwann cells and they change their behaviour. They now are cells that can encourage regeneration. So effectively what we would need to do is to build an artificial construct which had cells in it that could effectively do the same job as those supportive Schwann cells.
And the really important thing is that whilst neurons can regenerate given the right environment, they do it quite slowly which means you really need to organise the cells and the materials in such a way that it really will guide neurons directly from A to B. Of course the challenge as with all living cell therapy in regenerative medicine is where you actually get those Schwann cells from.
Katie - So where do you get them from?
James - Ideally we would just want some of the patients Schwann cells. The trouble is you can only get one cells from a patient's nerve and that would involve damaging the nerve. So what we've done over the last few years is explored other ways of getting cells that are either like Schwann cells or we can turn into Schwann cells.
So a few things that we've tried have been taking stem cells from different places, for example from fat tissue, bone marrow even from dental pulp within teeth and trying to turn those cells into Schwann cells or Schwann cell like cells and that can work reasonably well. But of course there are limitations with that. If you take a patient's cells maybe from their tissue and expand them in culture that takes a few weeks and you've no idea whether they're going to work properly.
The most promising cells that we've found are the idea of using what we call an allergeniac source of cells. So that means it's a source of cells that's from another patient. Effectively you could have them already prepared, build your constructs out of them. So as soon as the patient comes in they can be used off the shelf and implanted immediately into a patient who needs them.
Katie - What do these gels actually look like? And also I am guessing you need something to hold them together. So what are they bound by? Do they look like jelly?
James - The cellular materials we make are hydrogels, made of collagen and which is exactly what nerves are made of. They do look just like a very small jelly. We take a solution of collagen and we mix it with our cells and we put it into a mould and it sets. And then what happens inside there is that the cells will naturally interact with the collagen extracellular matrix and by controlling the tension that the cells produce we can actually then organise the cells to be nice and aligned in three dimensions. Typically the ones we make in the lab for experimental use are about 15 millimeters long and maybe a millimeter or two in diameter.
Katie - Once this has gone in to a patient or a model organism, would the idea be that the nerves will regrow, reconnect and then what happens to that gel?
James - Our approach tends to be to use a natural protein material. Effectively it integrates and then will become part of the body's protein and will be turned over by the body's cells in a natural way. I should add however that the cellular gel part of this is just like the middle of a nerve which is actually relatively weak. The thing that gives nerves their strength and resilience really is the kind of outer sheath part of it. So those need to be a bit stronger and a bit tougher generally so that they can withstand all the bending and stretching that's required. Now that part we probably wouldn't want that to dissolve or disappear too quickly, we'd want it to stay there. And again to integrate and become like natural nerve tissue.
Katie - Do you have any problems with things like rejection which seems to be a really big issue in regenerative medicine?
James - The response of the body is absolutely critical for this to succeed well when we really need to make sure that the materials themselves we put in will not be targeted and rejected quickly by the host immune system. One of the other important things of course is if you’re putting in dense cellular material, those cells if they don’t get oxygen and nutrients fairly soon then they're going to die. So actually what we need to do is to make sure that blood vessels grow into our artificial tissues as soon as possible, so that the cells we have implanted will survive. This is one of the things where we've teamed up with Becky's group because they're real experts in modelling and understanding what makes blood vessels grow into particular areas and how we can then design our artificial tissues to really exploit that.
Katie - So on that note, how do you actually design these gels?
Becky - So there's a lot of open questions really around how you should best design one of these repair constructs to encourage growth of neurons and growth of blood vessels through the repair sites. And those questions really come down to where you position the cells and where you position the materials to maximize the chance of a good repair. So we use computer based models to explore different kind of designs and try and predict which ones have the best chance. And then we use that to inform the experimental work in James's labs.
It's really quite fundamental components like for a start how many Schwann cells should we put in one of these devices in the first place and then where we should put them. So one of the really important components that we need to consider is this concept of gradients, so variations in different factors in space and neurons are very clever in being able to respond to these kind of spatial variations.
Katie - How far along are you with them?
James - We’re at a really exciting stage at the moment. For years the problem for us has been what's a realistic source of cells? Cell therapy technology has moved so fast in recent years and there's so many things available now. Our lead option is an off the shelf cell type that's already been used in the clinic to treat things like stroke and that gives us a really good starting cell because we know that it's got the right kind of safety profile and has been through some regulatory procedures, they've been in clinic in trials.
So what we've done is we've taken those cells and we've manipulated them a little bit and used them to build our artificial tissue and we've been testing that over the last few years in the lab and it's looking really quite promising. We've actually formed a company to take this forward, so joined up with some clinical partners and and commercial sector partners to really try and move this forward through regulatory approval, get some investment in. We've got to take the manufacturing forward.
Katie - Looking ahead how would you summarize the significance I guess of this artificial tissue in terms of a difference it could make to someone who has had a traumatic nerve injury?
James - Autograft sounds like a straightforward thing, you just find a nerve that's not really used much and chop it out and use that. But actually these you know it's a really major operation to strip out a section of nerve. There's always going to be damage of that donor site, scarring, extra time, extra cost for the operation but actually the big benefit would be the impact on the patient. The surgeon would only be repairing a nerve. They wouldn't also be having to damage what was previously a healthy nerve.
Becky - People who have peripheral nerve injuries have already got you know a very serious debilitating injury. So if we can find a way to try and repair that without having to cause them any further harm or further surgeries or further scarring that has the potential to make a real difference.










Comments
Add a comment